The life sciences and healthcare sectors rank among the world’s most tightly regulated industries, with a regulatory landscape that is constantly evolving. Globalisation, rapid advances in science and technology, and the drive to improve patient outcomes and safety have fueled ongoing changes. Patient and consumer expectations are becoming increasingly sophisticated and demanding, with a greater emphasis on personalised, patient-centric experiences and the sharing of information about conditions and treatments. In clinical research, trial participants are now viewed as collaborators rather than mere subjects.
Adapting to new regulatory requirements is crucial for companies’ commercial viability and reputation, and the ability to respond quickly and efficiently is vital. However, the transition can be challenging, especially for companies with fragmented systems and siloed data that now need to be aligned and integrated.
This paper focuses on the ever-changing regulatory environment in the medical devices industry and the corresponding obligations that medical device organisations must comply with. Although the in-vitro diagnostics (IVD) sector has also undergone significant regulatory changes, it falls beyond the scope of this paper.
Medidata has identified several key themes in managing medical device data that are crucial to advancing product development, driving innovation, and improving treatments for patients and consumers.
The International Regulatory Standards Landscape
The global medical device market is governed by a significant and wide-ranging plethora of international, regional, and national regulations as well as device and equipment standards. Medical device standards allow institutions in the medical device field such as product manufacturers, laboratories, and others to inspect and assess such equipment and devices to ensure standard quality and usability across the operators. Some standards (non-exhaustive) key to medical devices and clinical research are outlined below:
- ISO 13485 is used for establishing conformity with quality system requirements to demonstrate the consistent delivery of the medical device that has been approved by the regulatory authority. ISO 14971 has become the benchmark for a medical device risk management process. Again, there are multiple standards in use. Some standards would be used for all medical devices and other standards based on the device type.
- ISO 14155 Clinical investigation of medical devices for human subjects — Good clinical practice – ISO 14155 is essentially good clinical practice (GCP) for medical devices and has had an overhaul with the latest version published in July 20201. This standard is linked to other standards and regulations that address good clinical practice for the design, conduct, recording, and reporting of clinical investigations carried out in human subjects to assess the safety or performance of medical devices for regulatory purposes. This standard somewhat harmonises with the International Conference on Harmonisation (ICH) GCP guidelines for the pharmaceutical industry, i.e., ICH E6 R2 GCP. There are similarities and differences between the two but fundamentally both provide clear guidance on designing, conducting, recording, and reporting results from clinical trials designed to assess the safety, efficacy, and performance of drugs and devices products. The update to ISO 14155:2020 includes additions within the following areas:
- GCP principles
- Roles and responsibilities
- Clinical quality management, clinical investigation audits and ethics committees
- Risk-based monitoring requirements
- Clarifications on requirements applying to each stage of clinical development
- Annexes relating to EU MDR
- Data requirements in monitoring & across the life cycle of the device development
- Electrotechnical Commission (IEC) – There is aligned collaboration and cooperation among the International Electrotechnical Commission (IEC), the International Organization for Standardization (ISO), and the World Health Organizations (WHO), who develop international regulatory harmonisation initiatives to develop practical, effective and compliant medical device standards. IEC and ISO Standards are internationally recognized by medical device regulators. IEC prepares and publishes international standards for electrotechnology, such as the IEC 60601 which is widely recognized as the fundamental safety standard for medical electrical equipment. There are multiple standards with many common to any device but some are specific to the medical device being produced.
In addition to these international standards, there are certain requirements which are regional and nation-specific. Regulations and laws are not totally harmonised and vary between regions and countries. Navigating this can be a complex and time-consuming process.
Regional Perspective
UNITED STATES MEDICAL DEVICE DEVELOPMENT – REGULATORY PROCESS SUMMARY
In the US, the Food and Drug Administration (FDA) is the institution responsible for regulating medical devices.
The determination of medical devices is variable depending on the legislative region for market entry, but regulatory guidance is available to help navigate the decision-making process. The USA’s FDA makes resources available that help manufacturers understand whether a product is a medical device 2. The decision is based on intended use and indications, such as for example products intended to diagnose, cure, mitigate, treat or prevent disease, or affect the structure or function of the body while not achieving its primary intended purpose through chemical action and is independent of being metabolised. Once it is clear that a product falls within the scope of a medical device, the next step is understanding the appropriate applicable product classification. Software can also be classified as a medical device, including “Software as a Medical Device (SaMD)” and “Software in a Medical Device (SiMD)”, and a digital navigator 3 can be used to determine if a particular software is a medical device.
The FDA uses a risk-based classification system that groups medical devices into three categories, Classes I, II, and III. Class I is associated with the lowest risk and class III is the highest risk 4. The requirements for each classification vary. There are key regulatory areas that govern medical devices in the US, these are outlined below and not exhaustive:
- Establishment Registration & Medical Device Listing – Both manufacturers and distributors have to register with the FDA to be able to introduce their devices to the market.
- Premarket Notification 510(k) – Premarket notification is required for most, but not all medical devices. If a device requires the submission of premarket notification, it cannot be commercially distributed in the United States until it receives an authorization from FDA. The FDA has finalised its guidance on the “Electronic Submission Template for Medical Device 510(k) Submissions,” this will require medical device manufacturers 510(k) to use the FDA’s electronic Submission Template And Resource (eSTAR) format. This becomes effective as of October 1, 2023.
- Premarket Approval (PMA) Premarket Approval (PMA) is a risk-based evaluation process designed for devices that pose a high threat to patients’ health. Manufacturers of Class III devices (and devices that are not substantially equivalent to Class I or Class II) are required to submit a premarket approval application.
- Investigational Device Exemption (IDE) – allows manufacturers to use the device in question in clinical studies to collect evidence that proves its general safety and effectiveness. Data gathered during IDE-related studies is typically used to support a PMA.
- Quality System Regulation – The Quality System Regulation includes requirements related to methods, controls, and facilities used for the designing, manufacturing, labelling, packaging, storing, purchasing, installing, and servicing of medical devices.
- Labelling – Labelling regulations lay out the requirements for the labels on the device and the descriptive literature related to the device.
- Medical Device Reporting – Medical Device Reporting (MDR) has been established in order to help FDA and manufacturers identify and monitor the negative effects of a specific device in a timely manner. All deaths or serious injuries must be reported to the FDA under the MDR program.
- Unique Device Identifier (UDI) – The Unique Device Identification System, commonly referred to as UDI, is a Food and Drug Administration (FDA) rule that requires medical device labelers to mark medical packages and devices with a unique barcode 5. There are different compliance policies and rules for each device type. FDA has now published their updated
- policy regarding Global Unique Device Identification Database (GUDID) submission requirements for certain Class I devices considered consumer health products.
The FDA has been modernising some of these processes and requirements to ensure they keep up to speed with the rate of scientific and technological change.6
Due to an increase in violations over the past years, regulatory authorities have increased scrutiny of data integrity. The FDA defines data integrity as “the completeness, consistency, and accuracy of data which should be attributable, legible, contemporaneously recorded, original or a true copy, and accurate.” The integrity of data generated by medical device manufacturers is critical. Correctly recorded and complete information is the basis for manufacturers to ensure product identity, strength, quality, and safety. Data integrity builds the foundation for creating safe medical devices.
The FDA provides guidance and continues to focus on cybersecurity device design, labelling, and the documentation that it recommends be included in premarket submissions for devices with cybersecurity risk. This ensures that marketed medical devices are sufficiently resilient to cybersecurity threats.
In addition, Software as a Medical Device (SaMD) opens up new possibilities in healthcare. The healthcare industry is being transformed by this technological breakthrough, and there is an inclination toward deploying AI-ML-based technologies in the medical device field. The FDA’s Digital Health Center of Excellence has delineated an action plan 7 with operational guidance for both SaMD and software in a medical device (SiMD), which proposed a tailored regulatory framework for AI-ML-based SaMD, Good machine learning practice, Patient-centred approach incorporating transparency to users and Regulatory science methods related to algorithm bias and robustness.
Another example of regulatory modernization is the FDA’s Real-world evidence (RWE) program, a pivotal step in modernising the medical device industry by enabling the evaluation of medical devices’ safety and efficacy using real-world data (RWD) in addition to clinical trial data. The FDA’s RWE program also allows for continuous monitoring of medical devices using data from various sources and can rapidly identify potential safety concerns. By incorporating RWE, the FDA can evaluate the performance of medical devices across a diverse patient population and clinical settings. Medical device manufacturers can leverage existing RWD sources to reduce the time and cost of clinical trials, accelerating the regulatory process and facilitating quicker access to innovative medical devices for patients.
On December 29th, 2022, The Consolidated Appropriations Act was signed which included the Food and Drug Omnibus Reform Act, (FDORA). The legislation contains information under Chapter 2, ‘Mitigating shortages’, which includes information on the registration of foreign device manufacturers, combating counterfeit medical devices, and a section on preventing a shortage of medical devices 8. The bill also contains provisions on medical devices, including outlined scenarios for dual submission for certain devices, and ensuring cybersecurity in medical devices that can be referred to as cyber-devices, with cybersecurity vulnerability monitoring plans required.
MEDICAL DEVICES REGULATION IN THE EUROPEAN UNION
The regulation of the medical device industry in Europe has remained stagnant since the 1990s. However, prompted by numerous patient safety incidents and demographic shifts, such as an aging population9,10, regulatory reforms were introduced to improve the industry’s transparency, safety, and efficacy.
Among the most significant of these are the European Commission’s 2012 proposals for regulation on medical devices (EU MDR) and in-vitro diagnostics (EU IVDR).
- EU MDR Regulation (EU) 2017/745 of the European Parliament and of the Council of April 5, 2017, on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC.
- EU IVD Regulation (EU) 2017/746 of the European Parliament and of the Council of April 5, 2017, on in-vitro diagnostic medical devices and repealing Directive 98/79/EC and Commission Decision 2010/227/EU.
The EU MDR, building upon the previous Medical Device Directive 93/42/EEC (MDD), was adopted and implemented as of May 26, 2021, and has an increased emphasis on device safety. The regulatory framework provides transitional provisions, which enable medical devices compliant with the MDD to remain available in the EU market until May 26, 2024.
The European MDR classification system is similar in outlining medical device classes, ranging from low-risk class I, medium to high-risk class IIa, IIb, and high-risk class III13. The requirements for devices of higher risk are more stringent, for obvious reasons of safety.
However, due to COVID-19, as of April 2020 the European Commission14, has adopted a proposal to postpone by one year the date of application of the Medical Devices Regulation to allow Member States, health institutions, and economic operators to prioritise the fight against the coronavirus pandemic.15
As of February 2023, the European Parliament has officially approved the transitional period modifications following an overwhelming vote on a proposal by the European Commission . The proposal comes as a result of the risk of the original transition timelines potentially leading to medical device shortages, and an attempt to preserve patient access to medical devices . In the proposal, the European Commission acknowledges that despite great efforts, the capacity of conformity assessment notified bodies remains insufficient to meet the original transition timeline for the volume of medical devices16. If notified body approvals were to continue on the current trajectory, then all 8,120 devices can be transitioned from Directive to MDR certificates December 2027, and at the time of the writing of the proposal, only 1990 MDR certificates were issued of the total number, around a quarter of the total number, states the proposal.
The timeline for the transitional period now varies according to the risk classification of medical devices, depicted in the table below.
Table depicting the updated transitional periods for the European MDR.
| Class of Medical Device | New Transitional Deadline |
| “sell-off date”* | No Longer Applicable |
| Lower-risk: Class I/IIa/IIb | December 31, 2028 |
| Higher-risk: Class IIb/III | December 31, 2027 |
| Class III Implantable | May 26, 2026 |
*sell- off date has been removed, previously this was defined as “the end date for the further making available
The impact of these regulations and associated operational aspects has had a significant repercussion on the landscape for the operations of medical device manufacturers, importers, distributors, and health institutions and generally economic operators. Most organisations have been preparing for this transition for many years. The cost of compliance has been significant to prepare for and the reality of all this work to implement will only be proven well beyond a year from now.
The EU MDR, and the breadth of medical devices to which it applies, has been significantly expanded and includes certain products which previously did not fall under the definition of a medical device. Some key elements of the new legislation include:
- Enhanced vigilance and market surveillance: Once devices are available for use on the market, manufacturers are obliged to collect data about their performance, and EU member states will coordinate more closely in the field of market surveillance.
- Improving traceability of data – The EU MDR will ensure vital information is easy to find through more stringent traceability measures. For instance, patients will receive an implant card with all the essential information, and a unique device identifier will be mandatory for every product. A unique device identifier will be mandatory for every product.
- Transparency of data – the European Commission will establish a centralised European database for the storage of information on medical devices, this is called EUDAMED. EUDAMED is a multipurpose system structured around 6 modules concerning stakeholder and UDI registration, notified bodies and certification documentation, clinical investigations and performance studies, vigilance and market surveillance.This will facilitate the communication of both pre- and post- approval product information between economic operators, the Commission, EU Member States healthcare professionals, and the public.
- Clinical Performance Studies and Clinical Evidence: The EU MDR will require device manufacturers to conduct clinical performance studies and provide evidence of safety and performance, proportionate to the risk associated with a given device. The new EU MDR will lead to changes in the medical device development process due to new clinical evidence requirements. Additional clinical evidence will also be required for products already on the market. An understanding of the impact on R&D and the ability to retain products on the market and launch products in the pipeline will be crucial.
- Risk-based classification system: A new system has been developed for risk classification in accordance with international guidelines. While the classification system (Class III, Class IIa, Class IIb, and Class I) will be retained, some rules have been strengthened. This may result in a significant number of product types previously exempt from the regulations now being included in the scope.
- Post Market Surveillance System (PMSS): As part of their quality management system, manufacturers must also establish a PMSS, which should be proportionate to the risk class and the type of device in question. Manufacturers will have to report all incidents, injuries, and deaths into an EU portal that will contain relevant data, so patients have access to safety-related information.
- Greater enforcement and governance and tighter controls: The new requirements will impose tighter pre-market controls on high-risk devices and apply a more rigid approach to the conduct of both clinical evaluation and the clinical investigation of clinical trials. EU cross-border clinical trials will be subject to a single coordinated assessment. Stricter requirements on the use of hazardous substances will also be introduced, and device manufacturers will be required
- to collect and retain post-market clinical data, as part of the ongoing assessment of potential safety risks.The EU MDR is placing further responsibilities on the notified bodies, now being subjected to heightened scrutiny from competent authorities. Notified bodies have to be designated under the EU MDR, with the process of designation coordinated at a European level. In addition, notified bodies may pay unannounced audits to manufacturers.
- Introduction of an Expert Panel: under MDR’s Article 106 with the aim of an impartial and objective performance evaluation and device risks review, as the panel is independent of notified bodies and manufacturers
European Union Medical Device Approval Process
The EU medical device approval process is initiated when a foreign manufacturer designates a Person Responsible for Regulatory Compliance (PRRC), who acts as the primary liaison between the manufacturer, notified bodies, and national competent authorities. The sponsor must determine the category of the device in question.
For Class I, non-sterile, and non-measuring devices, a Quality Management System (QMS) is not formally required, though a Post-Market Surveillance (PMS) procedure is necessary, which is not audited by a Notified Body. For devices belonging to other classes, a QMS is required, and most companies seek compliance with the ISO 13485 standard. The manufacturer must prepare a technical file to demonstrate compliance. For class III devices, a dossier must be compiled. The QMS and technical file (dossier for class III devices) must be audited by a Notified Body. There is no audit or technical file required for class I, non- sterile, and non-measuring devices.
Medical device manufacturers must also prepare a declaration of conformity, with certificates issued by notified bodies being valid for a period indicated on the certificate, which cannot exceed five years according to Article 56 of the MDR. Should a notified body discover that any of the MDR requirements are not being met, the certificate of conformity will be suspended or withdrawn. The manufacturers of all medical devices in the EU must be prepared for audits and extensive post-market surveillance and must register with the Notified Body and register the Unique Device Identifier (UDI) on EUDAMED.
Impact of EU MDR on Medical Device Approval
The EU MDR has posed significant challenges to the medical device industry, primarily due to a shortage of designated notified bodies. This has resulted in a substantial increase in the duration and cost of reviews for re-certification, which at this early stage of embracing the newly introduced pathway for medical device approval, is posing a transitory challenge to the industry. However, similar to all new regulatory standards, the novel period of adjustment is usually a learning curve and becomes more familiar and less burdensome with time. The introduction of new regulatory frameworks is always accompanied by embracing innovation and the ambition to improve the health and safety of the population.
AI in Medical Devices
Artificial Intelligence (AI) is increasingly being adopted in the medical industry and recent technological breakthroughs have resulted in many medical devices incorporating AI functionalities. In the forthcoming future, AI will be regulated by a cross- sectoral EU AI Act17, which has been proposed and is expected to encompass a wide array of high-risk AI systems, such as those that are integrated into medical equipment. Beyond the legal framework governing AI devices, data-focused regulations such as the proposal for the European Health Data Space will enable manufacturers to access a wider range of health data from EU Member States, thereby facilitating the development of more effective devices.
The AI Act from the European Commission is a cross-industry regulation proposal that adopted a common position at the end of 202218. Some of the conformity assessments and further requirements that will impact medical devices with AI elements and their manufacturers and might result in duplicative compliance requirements to those already imposed by EU MDR. This medical device ecosystem needs to be carefully monitored, and industry is calling for alignment with sectoral legislation so as not to introduce duplicative assessments on medical device manufacturers, which is already subject to stringent regulations. In an ideal world the regulatory framework from cross-industry and the medical device industry should be complementary.
UK MEDICAL DEVICE REGULATION
The UK’s Medical and Healthcare Regulatory Agency (MHRA) is the authority responsible for medical device regulation, including market surveillance, decisions oversupply and marketing, as well as the designation and monitoring of UK conformity assessment bodies. Since the UK’s departure from the EU, the medical device regulatory environment, including device certification, conformity marking, and device registration have all been revised in Great Britain (England, Wales, and Scotland) under the secondary legislation of amendment of medical device regulation of 2019. As of January 2021, there have been significant updates on the path to market of medical devices in the UK. Whilst the European CE marking and certificates issued by EU-recognised notified bodies will be recognised in Great Britain until June 2023, the new UKCA (UK Conformity Assessment) marking is the updated route to market for medical devices entering the market, where UK Approved Bodies conduct conformity assessments.
Where the market launch plan includes both Great Britain and the European market, it is important to note that the UKCA marking is separate and is not recognised in the EU, where a CE marking is the equivalent requirement. Until 30th June 2023, both UKCA and the EU CE marking can be utilised to place a medical device on the Great Britain market, however, after July 1st, 2023, entering the Great Britain market will only be possible with the UKCA mark.
All medical devices will require MHRA registration as a prerequisite for entering the market in the UK. Where the medical device manufacturer is not established in the UK, the MHRA registration is to be facilitated by a manufacturer-appointed UK Responsible Person. Upon entry to the UK market, a vigilance report needs to be submitted to the MHRA as appropriate if device-related incidents occur.
For medical devices targeted for UK entry, it is important to be aware of the differences in requirements in Great Britain (which consists of England, Wales and Scotland) and Northern Ireland, the latter hosting a set of distinct rules under the Northern Ireland protocol22. As such, the EU MDR is applicable in Northern Ireland as of May 2021, and IVDR as of May 2022, and CE market is required for medical devices entering the Northern Ireland market. In specific cases, such as when a UK Notified Body is undertaking the conformity assessment, a Northern Ireland-specific UKNI indication would also be required23. Certain devices, such as custom-made devices and IVDs, would also require a timely MHRA registration prior to entering the Northern Ireland market. Great Britain-based manufacturers planning to enter the Northern Ireland market should also be familiar with the requirement to appoint a European or Northern Ireland-based authorised representative. In light of unfettered access provisions, Northern Ireland, even after the 30 June 2023 expiration of CE mark being accepted in the UK, Northern Ireland businesses may continue placing CE-marked devices on the UK market, granted they qualify as “Northern Ireland goods”24.
The UK’s MHRA aims to ensure the UK can be a globally recognised innovation area for software as a medical device. The software and AI as a medical device change programme of 2022 set out a roadmap for the introduction of additional clarity to the regulatory requirements applicable for software and AI algorithms, whilst prioritising patient protection25.
Clearly, having robust regulations and laws in place ensures the supply of quality consistent, safe, efficacious devices. The regulatory environment is dynamic and evolving; new standards and regulations are seeking to harmonise and simplify the rules simultaneously improving patient safety, product traceability, data quality, consistency, and transparency demanded by patients and the public.
REGULATORY COMMON THEMES – IT IS ALL ABOUT DATA!
Regulators are trying to keep pace with science and technology and there are common themes across the evolutions and there are solutions to address the changes. If you step back from the detailed guidance and consider the common themes in general there is an all-round greater emphasis on:
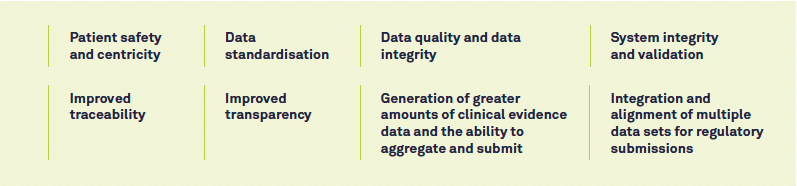
Typically, companies have several challenges when effectively leveraging data to foster product innovation.
Structuring and standardising data – Most data within a company and its associated ecosystem are fairly unstructured, which means it must be converted into structured data which can be a very manual resource-intensive process, prior to aggregation, integration, and analysis. Advances in statistical processes help clean and/or analyse unstructured data.
Combining multiple datasets – Integrating data from disparate datasets can provide novel insights. Managing data from different platforms and data streams can be overwhelming, extremely resource intensive, and costly. Errors and oversights can cause frustration, loss of valuable data, and even compliance issues.
Data ownership and privacy issues – Major concerns have been raised over privacy, confidentiality, and control of patients’ data once it is acquired. In general, individuals are increasingly concerned about data breaches, the implications of data analytics, and transparency over the control of data ownership. Furthermore, when it comes to the acquisition of data from a variety of sources, there are additional vulnerabilities regarding data privacy since the data are often accessed and utilised by a multitude of data scientists, often via vulnerable open-source technologies. Overall, these risks must be managed at the level of the medical device company.
Leveraging data to support auditing, regulatory inspections, and positioning commercially by:
- Capturing a wider variety of non-traditional clinical data derived as close to the source as possible, including electronic health records, imaging data, sensor data, and patient-provided data
- Establishing the ability to aggregate data quickly based on standards and governed data management
- Serving analytical reports and dashboards to the broad audience for analysis and collaboration
The huge volume of information demands an infrastructure that can assure that the data are reliable and not siloed.26
With rapid innovation in medical devices, it is essential that regulatory innovation follows. Globally regulatory agencies recognize the need for regulations to evolve and adapt, and these agencies are continually implementing new models to generate clinical evidence and other data sets to strengthen product quality while safely improving patient outcomes.
Having complete control and unification of data can help drive insights, facilitate and foster innovation and flex compliantly to a dynamic regulatory environment. Utilising big data in an efficient and meaningful manner requires up-front planning and
investment in the infrastructure and data alignment and integration. Once the appropriate infrastructure has been established, the struggles of dealing with huge volumes of information are minimised, and manufacturers can focus their efforts on bringing life-changing medical devices to market. The organisations with the best control of their data and unifying systems have the capability to provide faster insights and can accelerate product development faster – outpacing the competition.
Making this a Reality with Medidata
Medidata
Medidata, a Dassault Systèmes company, is renowned for its pioneering technological advancements in clinical trials, surpassing 30,000 clinical trials and 9 million study participants. Its cutting-edge Medidata Platform is the sole unified platform within the life science industry that covers the complete clinical research process from beginning to end. It prioritises precision medicine, sustainable innovation, and patient-centricity to ensure that Med device companies achieve clinical and long-term prosperity within a progressively intricate regulatory environment. It is the preferred platform of nine out of the top 10 medical device companies.
Medidata Clinical Cloud®
Medidata’s SaaS-based platform, the Medidata Clinical Cloud®, transforms and unifies the clinical trial experience for patients, sites, sponsors, and partners in a secure and scalable cloud environment. Designed as a unified data platform, with RAVE EDC (Electronic Data Capture) system as the cornerstone, the Medidata Clinical Cloud® creates a single source of truth for all study-related data, eliminating the need for multiple logins, data reconciliation, and spreadsheets. The impact of the Medidata Clinical Cloud is significant, as it offers an end-to-end unified platform solution, saving time and resources while improving patient outcomes.
Medidata Link
Medidata Link connects clinical trial data to US-based real-world data ecosystems at the patient level. It seamlessly integrates into existing clinical workflows, manages data linkage consent status, and centrally stores patient personally identifying information (PII) needed to generate de-identified tokens at scale. This allows for a longitudinal view of the patient journey and unlocks an array of otherwise-impossible analytics, including but not limited to: tracking long-term safety and effectiveness outcomes, monitoring patients lost to follow-up, and measuring the total cost of care. Medidata Link was recently awarded the 2022 Innovation Award from Reagan-Udall Foundation for the FDA.
Medidata Patient Cloud
Patient Cloud is a suite of powerful solutions designed to simplify and enhance the patient experience when participating in clinical trials. These solutions are built into the Medidata Clinical Cloud® platform, incorporating leading clinical trial technology with unmatched patient centricity by design. Patient Cloud offers a full range of scalable and flexible tools for every level of onsite and decentralized clinical trials. Their commitment to patient centricity is evident through the involvement of the Patient Insights Board, which consists of patients with real clinical trial experiences working alongside design teams to ideate, design, and certify products. The Patient Cloud suite of solutions include electronic informed consent (eConsent), electronic clinical outcomes assessments (eCOA), the data ingestion platform for wearable and biometric sensors (Sensor Cloud), a single sign-on patient portal for all trial activities pre, during and post-trial (myMedidata/ myMedidata Registries), all of which merge seamlessly into patients’ everyday lives, creating engaging interactions at every point of contact both virtually and on site.
Summary – A bRAVE/Bold New World
The Life Sciences and Healthcare industry is undergoing significant transformation as advancements in science and technology continue accelerating. As highly regulated sectors, it is crucial for regulatory frameworks to adapt and incorporate changes in a controlled manner to ensure patient safety and promote public healthcare.
Regulators are taking bold steps to modernise and update current frameworks amidst the constantly changing regulatory landscape, particularly considering the current global situation. The EU MDR regulations prioritise patient-oriented innovation and address the unique needs of small and medium-sized manufacturers in the sector. Clearer rules will facilitate harmonisation, standardisation, and more straightforward trading between EU member states.
In general, we are witnessing a regulatory revolution that seeks to modernise and enhance patient safety and public health by implementing greater oversight and monitoring, traceability, transparency, and a risk-based classification system for medical devices. Regulators are embracing innovation in medical device development and issuing new guidelines in several key areas.

A common underlying theme with many of the new regulatory requirements is about unlocking the power of the data and the execution of best-in-class data management procedures. This is multi-faceted, revolving around the use of standards to drive consistency and quality and the alignment and aggregation of quality data sets coupled with data analytics to drive insights. This is challenging with siloed data sources and disparate systems.
The organisations with the best governance and control of their data, with unifying collaborative infrastructures have the invaluable capabilities to provide faster insights and confidence through greater intelligence for decision-making. In turn, this can accelerate product development and agility to adapt to new regulatory frameworks – outperforming the competition and not just having a competitive advantage but also a high reputational public profile.
